Abstract
Venetoclax induces high rates of response (~80%), including complete remissions (CR) in patients with heavily pre-treated chronic lymphocytic leukemia (CLL) through inhibition of BCL2. Despite achieving deep and durable responses, most patients will eventually experience disease progression on treatment. The molecular mechanisms that mediate clinical resistance to venetoclax in vivo are largely unknown.
From a cohort of 67 relapsed CLL patients (Anderson et al, Blood 2017; 129:3362-3370) treated with venetoclax on three early phase clinical trials, we performed focussed genomic evaluation in those with CLL-type progressions (as opposed to large cell Richter's transformation). Targeted amplicon next generation sequencing of a panel of 33 genes recurrently mutated in lymphoid malignancy was performed where suitable pre- and post-progression samples were available. Twenty-one patients experienced CLL progression after a median of 36 months (range 6 - 73). Fifteen patients had paired samples for detailed analyses.
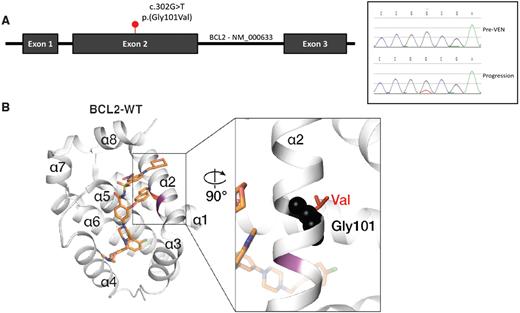
A single heterozygous nucleotide variant was detected in BCL2 (NM_000633.2:c.302G>T, p.(Gly101Val)) in progression samples in 7 of 15 patients (Fig 1A). Further investigation using a highly sensitive (limit of detection 0.01%) and specific droplet digital PCR (ddPCR) assay indicated that the Gly101Val mutation was first detected at low variant allele fraction after 19-42 months on venetoclax, up to 25 months earlier than when standard disease progression criteria were met. The Gly101Val was not detected prior to venetoclax treatment in this cohort and was not detected in a series of samples from patients treated at our institution who had not received venetoclax (CLL [n=74], NHL [n=198], myeloma [n=103]) nor has it been described in cancer (COSMIC) or population (gnomAD) databases.
To investigate whether Gly101Val directly causes resistance to venetoclax, we expressed it in two B-lineage cell lines (RS4;11 and KMS-PE-12). Gly101Val cells were ~30-fold less sensitive to venetoclax than cells expressing wild-type (WT) BCL2. The Gly101Val mutation conferred a selective advantage during continuous exposure to sublethal concentrations of venetoclax in 3-week cultures. The same phenomena was observed with primary patient Gly101Val mutant cells in both short-term survival assays and when cultured in a bone marrow stromal model (Thijssen et al, Haematologica 2015;100:302-6). On stroma, primary cells bearing the Gly101Val mutation demonstrated markedly increased resistance to venetoclax with concentrations higher than achievable clinically in vivo. In the absence of venetoclax, the Gly101Val mutant demonstrated preserved normal function by protecting cell lines from apoptosis induced by cytotoxics with similar effectiveness to WT BCL2.
In binding assays, the capacity for venetoclax to compete in vitro with BIM for binding to the Gly101Val mutant was markedly reduced (~180-fold) compared to WT BCL2. This is most likely explained by the presence of a bulkier valine residue in a region juxtaposed to the venetoclax binding groove (Fig 1B). In cell-based assays, whilst venetoclax readily displaced BAX and BAK from WT BCL2 it was ineffective when these pro-apoptotic molecules were bound to the Gly101Val mutant.
We observed that not all CLL cells at progression carried the Gly101Val mutation. One patient harbored distinct subclones with and without the BCL2 Gly101Val mutation at progression. The subclone with exclusively WT BCL2 was observed to have elevated BCL-xL by mass cytometry (CyTOF), while the Gly101Val clone had minimal BCL-xL expression. Together these data indicate that whilst the Gly101Val mutation is sufficient to enable clinical resistance to venetoclax, alternative mechanisms may also mediate resistance in the same patient.
In conclusion, we have identified and functionally characterized a novel recurrent BCL2 mutation (Gly101Val) emerging in a cohort of patients with CLL-type progressions treated with venetoclax. The BCL2 Gly101Val impairs binding of venetoclax to BCL2, confers resistance to venetoclax in both patient leukemia cells and engineered cell lines, and provides a selective growth advantage over wild-type cells when maintained in the presence of the drug in vitro. This mutation provides new insights into the pathobiology of venetoclax resistance and provides a potential biomarker of impending clinical relapse.
Anderson:Walter and Eliza Hall: Employment, Patents & Royalties; AbbVie, Inc: Research Funding; Genentech: Research Funding. Gong:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Thijssen:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Birkinshaw:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Teh:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Xu:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Flensburg:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Lew:Walter and Eliza Hall: Employment, Patents & Royalties. Majewski:Abbvie: Patents & Royalties: I am an employee of the Walter and Eliza Hall Institute which receives milestone and royalty payments related to venetoclax. Gray:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Tam:Gilead: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; BeiGene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pharmacyclics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Honoraria, Research Funding. Seymour:AbbVie: Consultancy, Honoraria, Research Funding; F. Hoffmann-La Roche Ltd: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Genentech Inc: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Honoraria, Research Funding; Celgene: Consultancy. Czabotar:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Huang:The Walter and Eliza Hall Institute of Medical Research: Other: Institutional funding for venetoclax including milestone and royalty payments.. Roberts:Walter and Eliza Hall: Employment, Patents & Royalties: Employee of Walter and Eliza Hall Institute of Medical Research which receives milestone and royalty payments related to venetoclax; AbbVie: Research Funding; Genentech: Research Funding; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal